Depression and anxiety are the most common mental health conditions worldwide, making them a leading cause of disability.
In recent years, the relationships between nutrition and mental health have attracted increased attention. Can food consumption choices impact your mood?
Over the past decade, researchers across the globe – from the US to Australia and the UK – have investigated potential links between vitamin D consumption, the Mediterranean Diet, and reduced symptoms of depression.
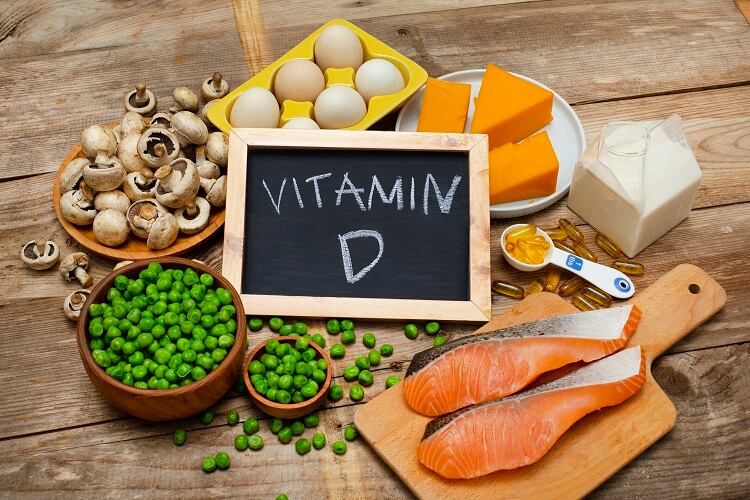
Vitamin D from food, rather than supplements, could improve mood
Vitamin D is both a nutrient we eat and a hormone our bodies make. The fat-soluble vitamin has long been credited with helping the body absorb and retain calcium and phosphorous – both important for building bones – and is thought to help control infections and reduce inflammation.
It has also been hypothesised that vitamin D may affect the function of dopamine and norepinephrine, which are monamine neurotransmitters that are likely involved in depression. Furthermore, vitamin D may modulate the relationship between depression and inflammation.
In 2011, a study published in The American Journal of Clinical Nutrition sought to determine whether vitamin D intake from food and supplements had an impact on depressive symptoms in postmenopausal women.
The list of foods that naturally contain vitamin D is a short one. The best sources are the flesh of fatty fish and fish liver oils, but smaller amounts are also found in egg yolks, cheese, and beef liver. Some mushroom varieties also contain vitamin D.
It is challenging to eat enough of the vitamin through food, and so for most people, the best way to get enough is through supplements.
A total of 81,189 females aged 50-79 years participated in the study. Vitamin D intake at baseline was measured by food frequency and supplement use questionnaires. Depressive symptoms at baseline and after three years were assessed by using the Burnam scale and current antidepressant medication use.
In cross-sectional analyses that used baseline data, women with the highest intakes of total vitamin D and vitamin D from food sources had a significantly lower prevalence of depressive symptoms as assessed with the Burnam scale compared with women who reported intakes of less than 100 IU (International Units) of vitamin D per day.
Further, in women without evidence of depression at baseline, a higher vitamin D intake from food sources was associated with a lower risk of depressive symptoms at year three.
Interestingly, the researchers did not find supplemental vitamin D intakes to be consistently related to measures of depressive symptoms.
“In conclusion, our results support an inverse association of vitamin D intake from foods and the occurrence of depressive symptoms in older women,” noted the study authors.
However additional studies, they stressed, are ‘essential’ for establishing whether vitamin D status holds promise for the depressions, the treatment of depression, or both.
Impact of the Mediterranean Diet on depression
Another study a few years later again focused on diet and symptoms of depression, but this time looking at the potential benefits of following a Modified Mediterranean Diet.
This diet is similar to the traditional Mediterranean Diet, which is high in vegetables, fruits, legumes, nuts, beans, cereals, grains, fish, and unsaturated fats, while also being low in meat and dairy.
The Modified Mediterranean Diet, created by Dr Rachelle Opie, recommends daily consumption of 5-8 serves of whole grains, 3 serves of fruit, 6 serves of vegetables, 2-3 serves of dairy, 60ml of olive oil, and 1 serve of nuts. Weekly, the diet recommends 3-4 serves of legumes, 3-4 serves of lean red meat, at least 2 serves of fish, 2-3 serves of poultry, and up to 6 eggs.
No more than 2 standard drinks should be consumed per day, exercise should be conducted daily, meals should be ‘enjoyed with others’, and plenty of water should be drunk.
Using a randomised controlled trial design, the researched aimed to investigate the efficacy of a dietary improvement programme for the treatment of major depressive episodes.
The 12-week, parallel-group, single blind, randomised controlled trial was known as ‘SMILES’ (Supporting the Modification of lifestyle in Lowered Emotional States). A total of 67 individuals with major depressive disorder participated.
Results were published in BMC Medicine in early 2017. After three months, all participants – from both the diet group and the control group – were assessed to compare with the baseline blood sample and notes on physical health, diet and mood. These last three parameters were again assessed six months later.
Results found that participants in the dietary intervention group had a much greater reduction in their depressive symptoms over the three-month period, compared to those in the control group.
At the end of the trial, a third of those in the dietary support group met criteria for remission for major depression, compared to 8% in the control group. Those who improved their diet experienced the greatest benefit to their depression.
The study authors suggested clinicians should also consider promoting the benefits of dietary improvement and facilitating access to dietetics support for their patients with depression.
How does mood impact food choice?
How mental wellbeing might be impacted by food consumption was more recently researched by Global Publish Health Nutrition MSc student Joanna Leeds during her time at the University of Westminster, UK.
The study, published in World Nutrition, sought to determine whether food choices had a positive or negative impact on the moods of 22 church-going women in inner London.
“We conducted individual interviews and focus groups with a sample of women of faith in inner London, in order to unveil key concepts surrounding their perceptions of food and mood,” noted Leeds at the time. “This exploratory study offered us a glimpse into women’s lives and their unique experiences relating to food choice and food-induced mood states.”

Findings revealed that women identified a number of internal and external factors as influencing their food choices and the effect of food intake on their moods. Food choice was influenced by mood; mood was influenced food choice.
Low mood was associated with unhealthy food consumption, apparent addiction to certain foods and overeating. Improved mood was associated with more healthy eating and eating in social and familial settings.
Leeds said she hoped findings from the study would contribute to the growing body of research surrounding food and mood.
Sources:
The American Journal of Clinical Nutrition
‘Vitamin D intake from foods and supplements and depressive symptoms in a diverse population of older women’
Published 24 August 2011
DOI: https://doi.org/10.3945/ajcn.111.017384
Authors: Elizabeth R. Bertone-Johnson, Sally I. Powers, Leslie Spangler et al.
BMC Medicine
‘A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial)
Published 30 January 2017
DOI: https://doi.org/10.1186/s12916-017-0791-y
Authors: Felice N. Jacka, Adrienne O’Neil, Rachelle Opie et al.
World Nutrition
‘Food and Mood: Exploring the determinants of food choices and the effects of food consumption on mood among women in Inner London’
DOI: https://doi.org/10.26596/wn.202011168-96
Published 24 March 2020
Authors: Joanna Leeds, Regina Keith, and Maria Woloshynowych.




