During July 2016-May 2017, the Alaska Division of Public Health (ADPH) investigated two outbreaks with five cases in each.
They were the first multiple-case outbreaks of walrus-associated trichinellosis in the state since 1992.
“Reasons for this decline in incidence are unknown and might involve changes in parasite burden in walruses; the timing or location of walrus hunting; methods used to store, collect, handle, or prepare walrus meat for consumption; reporting practices among ill persons; and clinical testing methods or practices,” said researchers.
Trichinellosis is a parasitic disease from eating raw or undercooked meat infected by roundworm species in the genus Trichinella.
The parasite cannot be reliably killed by smoking, drying or fermenting meat and the arctic species T. nativa is freeze tolerant.
Change in implicated food items
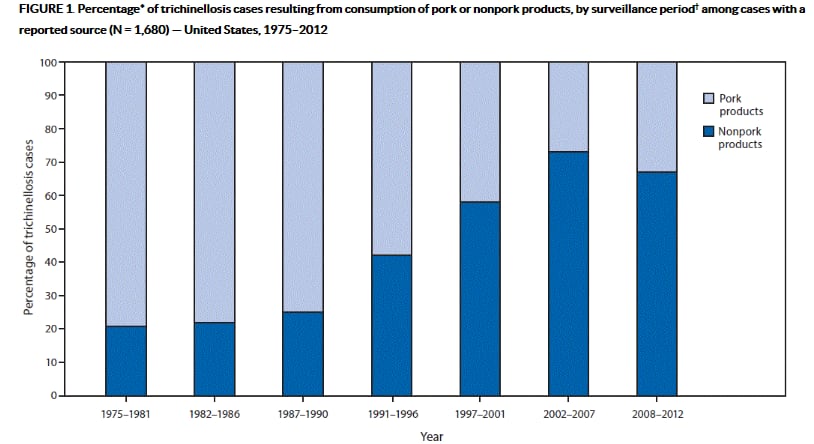
During 1975-2012, CDC identified 1,680 trichinellosis cases in the US with implicated food items; among these cases, 1,219 were attributed to raw or pork products and 461 to non-pork items.
Trichinellosis has historically been most frequently associated with raw or undercooked pork; however, non-porcine wild game species are now collectively implicated in the majority of US cases.
Walruses, polar bears and sea ice–associated seal species are important for the nutritional, cultural, and economic well-being of many coastal communities in northern and western Alaska.
In the first outbreak three patients ate raw or pan-fried (to “medium” doneness) walrus meat.
Serologic tests from two of them were positive for Trichinella immunoglobulin G (IgG) by enzyme-linked immunosorbent assay (ELISA).
Two additional suspected trichinellosis cases reported symptoms beginning about one week after consuming raw walrus meat. All five patients fully recovered.
ELISA testing identified IgG antibodies to Trichinella in one of them.
Leftover walrus meat was not available to test for Trichinella larvae and investigators could not determine when the walrus had been harvested, how widely associated meat had been shared or whether all five patients had meat from the same animal.
In the second outbreak ADPH was notified of another suspected case of walrus-related trichinellosis in a second Norton Sound coastal community, <100 miles from where the first outbreak occurred.
Blood tests revealed eosinophilia and elevated creatine kinase levels but Trichinella IgG results by ELISA were negative.
Interviews by ADPH and the Nome Public Health Center identified four other suspected cases based on reported illness or likely exposure via a shared meal of undercooked walrus meat in April.
Two patients had positive Trichinella IgG results by ELISA and two were negative.
“Given the high eosinophil counts and creatine kinase levels measured for the three patients with probable trichinellosis, it seems likely that these persons were infected but tested negative for Trichinella IgG by ELISA because the time elapsed between infection and testing was insufficient for a measurable humoral response,” according to the study.
Walrus eaten during the implicated meal in the second outbreak had been harvested and butchered during the previous one to three months and stored frozen in unlabelled bags in household freezers.
Meat was boiled for one hour, after which the exterior was fully cooked, but the interior remained undercooked or raw, which was the desired result. No meat from the meal was available for testing.
Positive sample and public health messaging
A convenience sample of meat from 11 bags was sent to CDC’s Division of Parasitic Diseases and Malaria’s service for laboratory testing.
One sample was positive for larvae of Trichinella spp. using differential interference contrast microscopy and polymerase chain reaction (PCR) with primers specific to internally transcribed spacer regions 1 and 2. The parasite was determined to be T. nativa by sequencing PCR products.
Researchers said the outbreaks highlight the importance of culturally sensitive public health messaging.
“In areas where wild game species are harvested for subsistence, traditional methods of collecting, handling, preparing, storing, and consuming meat often have great cultural significance; however, some of these methods can be inconsistent with public health best practices.
“These outbreaks underscore the importance of inquiring about consumption of commercially prepared and personally harvested meats, and about methods of meat preparation, when evaluating suspected trichinellosis cases, especially in areas where consumption of wild game in association with recreational or subsistence hunting is common.”
Source: MMWR Morb Mortal Wkly Rep 2017; 66:692-696
“Two Outbreaks of Trichinellosis Linked to Consumption of Walrus Meat - Alaska, 2016–2017”
Authors: Springer YP, Casillas S, Helfrich K, et al
