‘Alarm bells should be ringing’, following a report by the European Centre for Disease Prevention and Control (ECDC) and European Food Safety Authority (EFSA), said Vytenis Andriukaitis, EU Commissioner for Health and Food Safety.
Limited options
The research claims resistance to fluoroquinolones (such as ciprofloxacin) is so high in Campylobacter bacteria in some countries, antimicrobials no longer work when treating severe campylobacteriosis cases.
Salmonella in humans is becoming resistant to fluoroquinolones in most countries today and in Campylobacter, high to extremely high proportions of bacteria are resistant to ciprofloxacin and tetracyclines.
This means thousands of patients across the EU have limited options when it comes to treating severe infections.
Antimicrobial resistance
AMR is the ability of microorganisms to become increasingly resistant to an antimicrobial to which they were previously susceptible. AMR is a consequence of natural selection and genetic mutation. Natural selection is exacerbated by human factors such as inappropriate use of antimicrobials in human & veterinary medicine, poor hygiene conditions, and practices in the healthcare or food chain.
Andrea Wurz, health communication specialist, (ECDC), said the joint ECDC-EFSA report on antimicrobial resistance (AMR) in zoonotic and indicator bacteria from humans, animals and food, is based on 2017 data.
“AMR (antimicrobial resistance) in zoonoses shows no signs of slowing down and the antimicrobials used to treat diseases that can be transmitted between animals and humans, such as campylobacteriosis and salmonellosis, are becoming less and less effective,” she said.
Zoonoses are infections that are transmissible between animals and humans.
FoodNavigator published ‘The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2016’, highlighting emerging issues and claiming AMR is one of the biggest threats to public health.
“This year’s update refers to 2017 data; the findings are not significantly different from last year but confirm the situation is not improving. The fact that in several countries some antibiotics have stopped working altogether is not new but is persistent,” added Wurz.
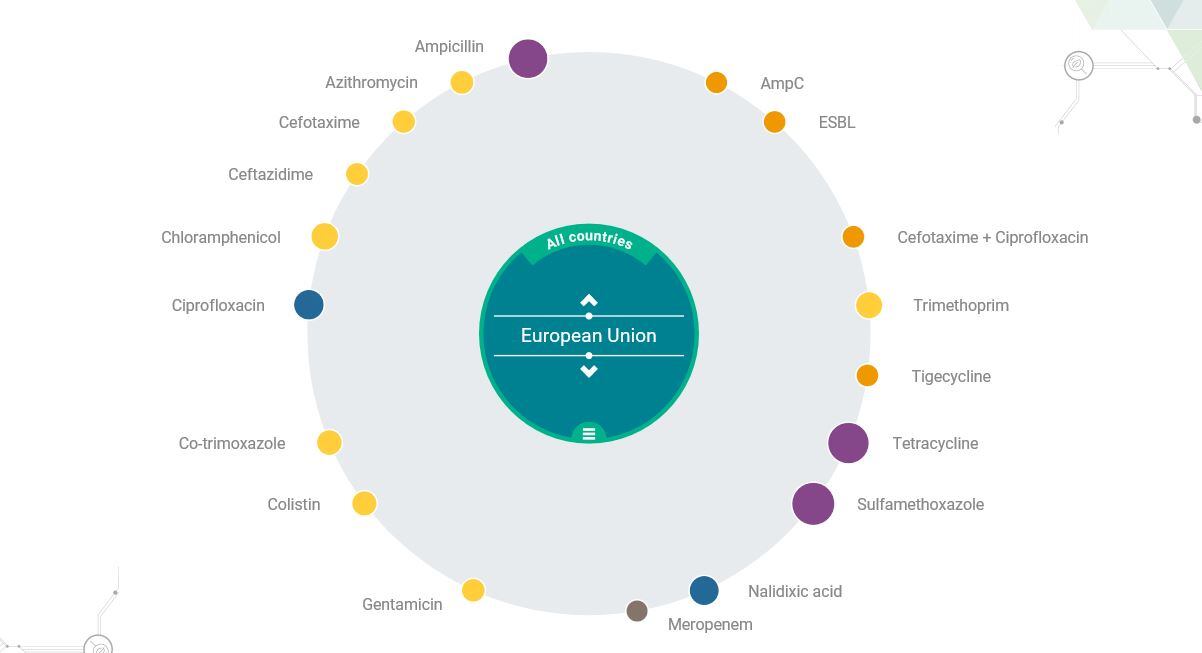
EFSA has also created an interactive infographic where consumers can analyse per country, per source (human/animal) and per antibiotic.
Bacterial resistance to antimicrobials in food-producing animals can spread to people via food-borne routes, water, environmental contamination, or through direct animal contact. Campylobacter, Salmonella and some strains of Escherichia coli are examples of zoonotic bacteria that can infect people by the food-borne route.
The report claims infections with bacteria that are resistant may result in treatment failures or lead to second-line antimicrobials for therapy.
The commensal bacterial flora can also form a reservoir of resistance genes, which may be transferred between bacterial species, including organisms causing disease in humans and animals.
Laboratory methods
"The main issues when comparing AMR data originating from different countries are the use of different laboratory methods and different interpretive criteria of resistance. These issues have been addressed by the development of ECDC’s protocol for harmonised monitoring and reporting of resistance in humans and recent legislation on harmonised monitoring in food-producing animals and the food produced," the report says.
The data on antimicrobial resistance in zoonotic and indicator bacteria in 2017 was submitted by 28 EU Member States from humans, pigs and calves under one year of age.
Varying occurrence/prevalence rates of presumptive extended-spectrum beta-lactamase (ESBL)/AmpC producers in Salmonella and E.coli in pork and beef, fattening pigs and calves, and Salmonella monitored in humans were observed between countries.
Carbapenemase-producing E.coli were detected in one single sample from fattening pigs in one Member State. Resistance to colistin was observed at low levels in Salmonella and E.coli from fattening pigs and calves and meat and in Salmonella from humans.
In Campylobacter from humans, high to extremely high proportions of isolates were resistant to ciprofloxacin and tetracyclines, particularly in Campylobacter coli.
In five countries, high to very high proportions of C. coli from humans were resistant to erythromycin, leaving few options for treatment of severe Campylobacter infections.
High resistance to ciprofloxacin and tetracyclines was observed in C. coli isolates from fattening pigs, whereas lower levels were recorded for erythromycin.
Combined resistance to critically important antimicrobials in human and animal isolates was generally uncommon but very high to extremely high multidrug resistance levels were observed in S.Typhimurium and its monophastic variant in humans and animals.
The report states: "Most countries reported that Salmonella in humans is increasingly resistant to fluoroquinolones. Multidrug resistance (resistance to three or more antimicrobials) is high in Salmonella found in humans (28.3%) and animals, particularly in S. Typhimurium.
"In Campylobacter, high to extremely high proportions of bacteria were found to be resistant to ciprofloxacin and tetracyclines. However, combined resistance to critically important antimicrobials was very low to low in Salmonella and Campylobacter from humans and animals and in indicator E. coli from animals."
One Health
“Now is the time to turn the tide on antimicrobial resistance if we want to keep antibiotics working,” said Mike Catchpole, chief scientist, ECDC.
“It’s particularly worrying when it comes to combined resistance: even low proportions mean many thousands of patients across the EU have limited treatment options for severe infections.”
Andriukaitis added: “We are entering into a world where more and more common infections become difficult–or even sometimes impossible–to treat. However, ambitious national policies in some countries limiting antimicrobial use have led to a decrease of antimicrobial resistance. So before the alarm bells become a deafening siren, let’s make sure we increasingly act all together, in every country and across the public health, animal health and environment sectors under the One Health approach umbrella.”
The European Commission adopted a new Action Plan to tackle AMR on June 29, 2017. The Action Plan is underpinned by a One Health approach that addresses resistance in both humans and animals.
The three key objectives of this plan are; making the EU a best practice region by promoting prudent use of antimicrobials, enhancing cross-sectorial work, improving infection prevention and consolidating surveillance of AMR and antimicrobial consumption.
Examples of support include providing evidence-based data with the support of EFSA, European Medicines Agency (EMA) and ECDC. Updating EU implementing legislation on monitoring and reporting AMR in zoonotic and commensal bacteria in farm animals and food and taking into account new scientific development, mutual learning, exchange of ideas and consensus building.
The second objective is boosting research, development and innovation by closure current knowledge gaps, and providing ways to prevent and treat infectious diseases and improving diagnosis to control the spread of AMR.
The third objective is intensifying EU effort worldwide to shape the global agenda on AMR and the related risks in an increasingly interconnected world.
The new plan includes more than 75 concrete actions with EU added value that the EU Commission will develop and strengthen as appropriate in the coming years. All these actions are interdependent and need to be implemented in parallel to achieve the best outcome.
Source: EFSA & ECDC
Date: 31/01/19
DOI: 10.2903/j.efsa.2019.5598
Requested by: The European Commission
Question number: EFSA-Q-2017-00752